Ever wondered what to say or not say to someone with depression? If you’re here, you probably care deeply about someone struggling, but you might worry about making things worse by saying the wrong words.
Helping a Depressed Person well doesn’t require perfect language, it just takes empathy, care, and the right approach. In this guide, you’ll find practical tips on how to support someone safely, common mistakes to avoid, and trusted resources you can turn to when things feel heavy.
Disclaimer: This post is for educational and emotional support purpose only and is not a substitute for professional help. If someone is in crisis, or if you feel overwhelmed yourself, please reach out to a qualified mental health provider or local emergency services immediately.
Table of Contents
ToggleWhat Is Depression?
Depression, often called major depressive disorder, is more than just feeling sad. It’s a serious mental health condition that affects feelings, thoughts, and daily functioning. People-first language helps us remember that depression is something someone experiences, not who they are.
The World Health Organization estimates that around 5% of adults worldwide or about 280 million people suffered depression in 2019. The prevalence rises to about 5.7% in adults over 6, with women slightly more affected than men.
According to the National Institute of Mental Health, about 21 million people (8.3% of adults) in the United States had at least one major depressive episode in 2021. Young adults (18–25 years old) have the highest rates (18.6%), with women experiencing a rate of 10.3% and men 6.2%.
From 2021 to 2023, CDC data shows that in any two-week period, 13.1% of people aged 12+ reported depression symptoms. That includes nearly 19.2% of teenagers, dropping to 8.7% in adults over 60, with higher rates among lower-income groups and females overall.
If you’d like more detail on symptoms or causes, check out my full guide on Understanding Depression.
Identifying Symptoms in a Loved One
Depression can look different from person to person. Spotting the early signs that can be emotional, behavioral, and physical can help you reach out before things become overwhelming. Here’s what to watch for:
- Emotional: Persistent sadness, hopelessness, irritability, numbness, or withdrawal from people and passions.
- Behavioral: Losing interest in hobbies or socializing, skipping work or school, difficulty with personal care like hygiene, and slowing down speech or movement.
- Physical & Cognitive: Chronic fatigue, frequent aches, changes in appetite or sleep, difficulty concentrating, memory slips, or indecision.
These signs can vary widely, as not everyone shows every symptom, and some people might show symptoms differently depending on their age, culture, or life stage. For example, older adults often have more physical symptoms like aches and sleep issues, which may mask the emotional side of depression.
Globally, depression remains a leading cause of disability, affecting millions across all ages and walks of life, highlighting how common and urgent this issue is.
Helping a Depressed Person: What to Do
Over my years as a psychologist, I’ve learned that the first words you say when you’re gently reaching out matter more than you might think. Here’s how I recommend beginning those delicate conversations, based on real practice, not just theory:
How to Start the Conversation
- Pick the right time and place: Choose a comfortable, uncluttered space and a calm moment when neither of you is rushed. Trust my experience; conversations flow better when both people feel safe and unhurried.
- Use “I” statements: Say things like, “I’ve noticed you seem sad or distant lately,” rather than “you’re depressed.” This keeps the tone caring, not accusatory.
- Ask questions; don’t give advice. Instead of saying “You should…”, ask open-ended things like, “Do you want to share more about how today felt?” It opens the door without pushing.
- Be present and listen: Give your full attention, put your phone away, and let them share without interruption. Maintain eye contact, nod, and give reassuring body language to show you truly care. In therapy, listening with empathy is one of the most powerful support tools available.
- Validate struggles as real: I explain that depression isn’t a choice or phase, it’s a real condition. Phrases like “It’s understandable to feel this way” help them breathe easier and lower defenses
- Offer gentle reassurance and shared hope: Something as simple as “You don’t have to do this alone” can be a lifeline. I’ve seen it open people up more than any pep talk ever could.
- Watch your tone and energy: In therapy, I also mirror emotions, using a slow cadence, soft tone and calm posture. It sends a subconscious message that you’re safe to slow down too.
Sample Open-Ended Conversation Starters
Here are some gentle phrases you might want to use or modify while helping a depressed person:
- “I’ve been thinking about you. How have you been feeling these days?”
- “I care about you and want to understand what’s on your mind.”
- “I’m concerned about you. Would you like to chat over a walk or coffee sometime?”
- “If it ever feels overwhelming, I’m here. Always.”
- “I can’t pretend to know exactly how you feel, but I’m here to understand as best I can.”
- “Depression is tough. You don’t have to go through this alone.”
- “I’m here to help whether it’s to find someone to talk to or just sit quietly with you.”
These approaches work when helping a depressed person because giving them a safe space to express tough feelings without judgment can actually shift their mood bit by bit. Feeling genuinely heard instead of pushed to fix things can be deeply healing. And by acknowledging hesitation and showing patience, you help someone trust you more quickly, laying the foundation for real support.
Practical Help
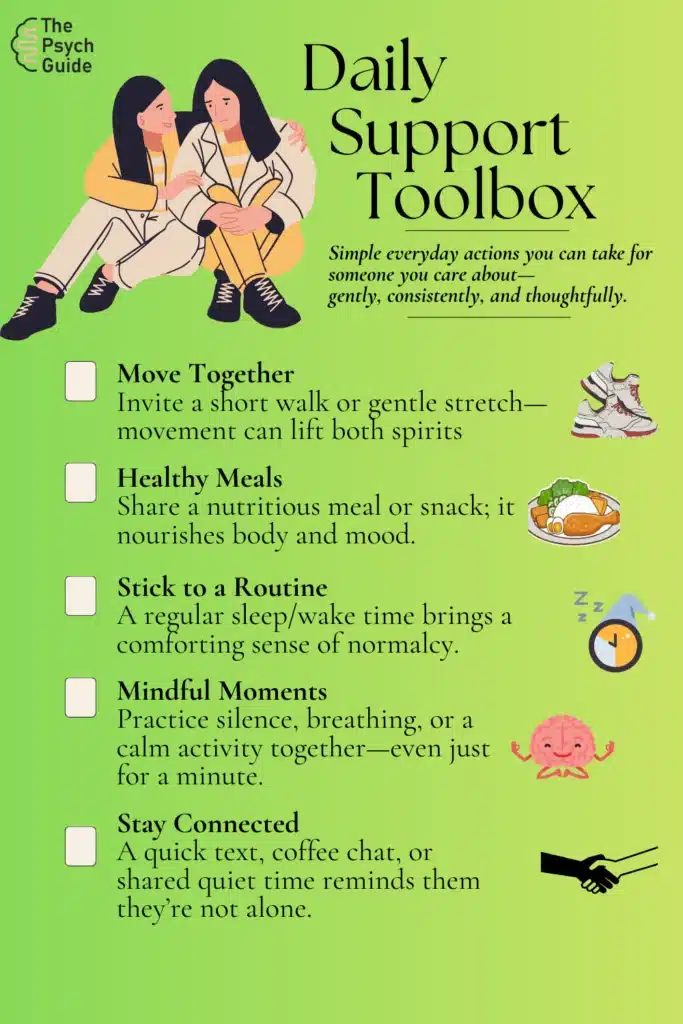
Providing emotional and practical help is central to helping a depressed person and even small efforts can have a big impact.
- Offer help with daily tasks: Chores, errands, cooking, or organizing bills can feel overwhelming. Assist in small ways that reduce their stress, such as taking on a task or sharing it together. Even sorting paperwork or preparing a basic meal can lift a bit of weight.
- Invite gentle activities: Depression often shuts down motivation but things like a short walk, sitting outdoors, or working on a hobby together (even quietly) can gently boost mood. You don’t need big events; you just need some time spent together.
- Encourage small steps (behavioral activation): Help them break down bigger tasks into small steps: maybe “sit outside for 10 minutes” or “drink a full glass of water.” These small wins slowly build momentum.
- Check In Consistently: A daily message or short check-in, even if they don’t reply, reassures someone you care. Consistency is often the most subtle part of helping a depressed person.
Encourage Professional Help
- Normalize therapy and medical treatment: Frame it as a normal and effective path to understand what’s going on and to find tools that work. For many, therapy or medication in combination helps recovery.
- Make help easier to access: Offer to research local providers, schedule appointments, or drive them if needed. Sometimes, people with depression struggle even to initiate these steps so your support here can be critical.
- Provide resources and crisis support info: Share trusted hotlines or directories like local helplines or online therapy referrals without pressuring them to use them immediately. Knowing they’re available helps.
By combining gentle emotional connection with practical support and guiding them toward professional help, you create a safe space and forward momentum. You’re not fixing everything, but you are making a visible difference in helping a depressed person feel less alone and better cared for.
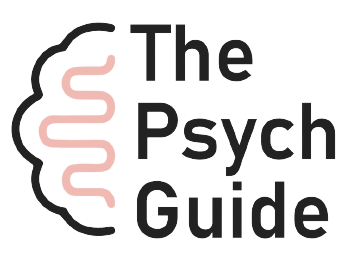
What Not to Do When Helping Someone with Depression
When you are committed to helping a depressed person, unintended mistakes can sometimes happen, which can hurt the person. Being mindful of these is key to creating a safe, compassionate space:
- Never dismiss their feelings with phrases like “You’re fine” or “Pull yourself together.” This invalidates their experience and increases feelings of isolation.
- Do not rush or put undue pressure on them by asking them to “just be positive” or “snap out of it.” It puts unfair expectations on their healing process and erodes trust.
- Avoid dominating conversations or acting like their therapist, offering solutions instead of listening. It undermines their autonomy and can feel patronizing.
- Never take their reactions personally, like when they withdraw or cancel plans. These behaviors are often symptoms rather than reflections of their relationship.
- Do not ignore your own limits and neglect self-care. Overextending yourself can lead to burnout and reduce your ability to be present.
Recognizing Suicide Risk
When you’re helping a depressed person, it’s important to also recognize when depression may cross into crisis. Suicidal thoughts or behaviors are not a sign of weakness; in fact, noticing them early and responding can make all the difference.
Here’s what to look out for:
- Talking about death, expressing guilt, or feeling like a burden
- Withdrawing from others, giving away cherished items, or settling affairs
- Shifts in mood—like swinging from deep despair to sudden calm
- Reckless behavior, substance misuse, or other impulsive actions
- Saying they feel trapped, hopeless, or without purpose
If these signs appear, it’s time to act; not wait or guess:
- Ask directly, but gently: “Are you thinking about ending your life?” This doesn’t plant ideas; in fact, research shows it helps people open up.
- Stay present and calm; let them know you’re here for them—without judgment or pressure.
- Reach out for help immediately if they mention a plan or intent: contact emergency services, a trusted mental health professional, or crisis hotlines like 988 (U.S.) or local services in your country.
Want to understand more about how depression links to suicide risk? Dive deeper into our full piece: [Is Depression a Leading Cause of Suicide?]
Prioritize Your Well-Being While You Support
Caring for someone with depression is a powerful act yet it can also drain you. If you’re helping a depressed person, remember: you deserve care too.
Here are a few quick things you can do:
- Give yourself permission to rest—even brief breaks help you recharge and return feeling more patient and present.
- Practice self-compassion—you’re doing hard, meaningful work. A little kindness toward yourself sustains your ability to help.
- Use simple stress-busters—try deep breathing, brief walks, or quiet time to activate your body’s natural relaxation response.
- Create boundaries—it’s healthy to say something like, “I need a little time to breathe and will come back refreshed.” Setting boundaries protects your energy so you can continue offering genuine support without burning out.
Taking care of oneself isn’t self-indulgence—it’s essential. You can support others, especially a depressed person, more effectively when your own needs are taken care of.
Conclusion
In the end, helping a depressed person isn’t about grand gestures; it’s about showing up with presence, understanding, and tiny acts of care that say, “You matter, and I’m here.” From listening with empathy, to sitting through the silence, to celebrating small steps forward, every effort chips away at the heaviness.
If you’ve read this far, you’re already showing incredible compassion. Your thoughtfulness matters because in the journey of helping a depressed person, consistency, kindness, and hope often matter more than perfection.
If you found this guide helpful, you might also enjoy these related reads:
- Interesting Facts About Depression – dig deeper into myths and truths.
- Depression: Types and Symptoms – useful for understanding what someone might be experiencing.
I’d love to hear how this helped you or someone you care about. Feel free to share your experience in the comments below or sign up for updates if you’d like tips delivered straight to your inbox.
Frequently Asked Questions (FAQs)
What three methods treat depression?
There are three main approaches: structured talk therapies (like CBT or IPT), antidepressant medications, and general wellness measures like relaxation, exercise, and lifestyle modifications. Often, a combination of these offers the best outcomes.
How to respond when help is refused?
Respect their boundaries and simply say, “I’m here when you’re ready.” Keep offering small gestures of care like “thinking of you” messages and gently revisit asking again later without pressure.
How to handle a depressed person?
Approach with empathy; listen, validate, offer small practical help and avoid judgment. Encourage healthy routines and professional care gently without pushing. Consistent, caring support builds trust over time.
What to say to someone that is depressed?
Phrases like “I’m here to listen if you want to talk”, “You don’t have to be okay right now,” and “What you’re feeling is real and valid,” offer understanding, comfort, and emotional safety.
What are words of encouragement for a depressed person?
You can say: “You are not your illness.”, “This too shall pass.”, “Every day may not be good, but there’s something good in each day.” These help inject hope and reinforce that their feelings don’t define them.